The safety of health care workers is critical to our response to COVID-19.
Updated information from Fraser Health Infection Prevention and Control on COVID-19 is available on Fraser Health Pulse. (Note: internal link - must be signed in to the Fraser Health network to access.)
-
How should we be washing our own scrubs/uniforms at home? Will the germs contaminate our washing machines?
COVID-19 like many other pathogens is killed by use of soap and water. Laundering used uniform/scrubs/other work clothing at home in the regular wash hot water cycle and tumble-dry is acceptable and will kill COVID-19 and will not contaminate your washing machine.
-
Can scrubs be issued to all health care areas?
In addition to the areas that normally receive scrubs, they are being issued to those areas that are caring for positive and suspect COVID-19 patients on the cohort units.
-
What’s the difference between a procedure mask and a surgical mask?
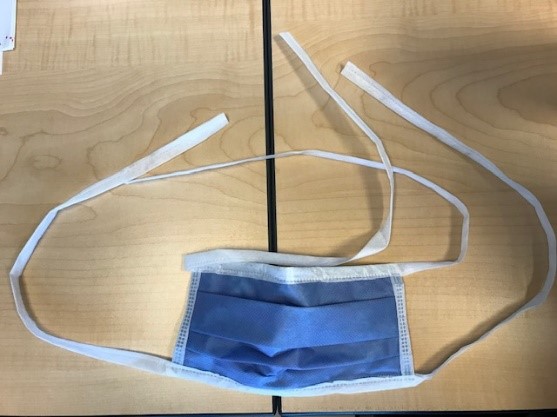
Procedure masks come with ear loops that are quick to don and doff for every day use in patient care areas. Surgical masks are meant to be used where surgical procedures are performed (ex. OR, ADC, cath labs). Surgical masks come with ties to be tied overtop surgical or bouffant caps and adjusted for a close fit.
Procedure mask Surgical mask 
-
What do the different levels of procedure masks mean?
Masks used in Fraser Health generally follow the ASTM F2100 standards. All rated procedure/surgical masks provide sufficient protection for droplet precautions (including COVID-19 patients).
The current ASTM standard specifies performance requirements for the material used in masks with five basic criteria:
Level 1
Level 2
Level 3
Bacterial filtration efficiency, %
≥ 95
≥ 98
≥ 98
Differential pressure mm H20cm2 (Pa/cm2)
<4.0
<39.2
<5.0
<49.0
<5.0
<49.0
Submicron particulate filtration efficiency at 0.1 micron, %
≥ 95
≥ 98
≥ 98
Splash resistance/synthetic blood resistance, mmHg
80
120
160
Flame spread
Class 1
Class 1
Class 1
An alternative standard considered acceptable by the government of Canada for COVID-19 response is the EN 14683 standard. This is an European standard with multiple “types” of masks (instead of multiple “levels”). There are three Types: Type I, Type II, and Type IIR. Only Type IIR is acceptable as it is the only one with splash resistance tested.
Test
EN 14683
Type IIR
Bacterial filtration efficiency, %
≥ 98
Differential pressure mm H20cm2 (Pa/cm2)
<5.0
Submicron particulate filtration efficiency at 0.1 micron, %
Not required
Splash resistance/synthetic blood resistance, mmHg
120
(16.0kPa)Flame spread
N/A
-
How do I choose the right level of procedure mask?
Selection of the most appropriate mask must be based on the risk of blood and body fluid exposure anticipated for the patient care needed. The biggest difference between the three ASTM levels is the splash resistance. There is increased fluid resistance with Level 2 and Level 3 masks and these should be used for tasks where higher amounts of fluid exposure and risk of splash are present.
The chart below can assist you in making this decision:
Level 1 (80 mmHg)
Level 2 (120 mmHg)
Level 3 (160 mmHg)


Pressure correlation
Venous pressure
Arterial pressure
High pressures that may occur during trauma, surgeries, etc.
Risk of splash
Low
Medium
High
Uses
Can resist splash or spray at venous pressure. Suitable for short procedures and exams that don’t involve (or minimal) spray or fluids.
Can resist splash or spray at arterial pressure. Suitable for low-to-moderate levels of sprays and fluids.
Have the highest fluid resistance. Suitable for heavy levels of sprays and fluids.
Tasks*
Procedure
- General bedside procedures
- Examination
- Simple wound care
- Respiratory etiquette
- General dental procedures
- Procedures with moderate risks of splash (ex. inserting arterial line, inserting central venous line, starting hemodialysis, upper GI endoscopy, uncomplicated vaginal delivery)
- High risk procedures (ex. complicated vaginal delivery, procedures in emergency department to control bleeding)
- High risk dental procedures (ex. use of air polisher, ultrasonic scaler)
Surgical
- General bedside procedures in PAR
- Transporting patients
- Tasks not directly involved with surgery or other procedures with risk of splash (ex. routine tasks by holding bay nurse, circulating nurse)
- Surgical procedures with low risk of splash (ex. intraocular injection, robotic surgical procedures, minor surface suturing)
- Procedures with moderate risks of splash (ex. inserting arterial line, epidural)
- Surgical procedures with moderate risk of splash (ex. minor local procedures such as biopsy and abscess drainage, insertion of contraceptive devices, locally anesthetized ophthalmologic surgery, laparoscopic procedures)
- High risk procedures
- Surgical procedures with high risk of splash (ex. open heart surgery, AAA, orthopaedic surgery, C-section, transplant, craniotomy)
- General oral surgery
*Examples of tasks – not an exhaustive list*Any AGP requires use of a filtering facepiece respirator (e.g. N95) or equivalent respirator (fit-tested within past one year) -
How do I keep my mask from getting wet, when showering/bathing patients?
Use a faceshield in addition to your procedure mask, to prevent it from getting wet while showering/bathing patients. Anti-fog sprays or wipes can be used to prevent the faceshield from fogging up. Other ways to reduce the steam produced are to reduce the temperature of the water or consider an alternate method of bathing i.e. sponge bath.
Anti-fog wipes (Soap Castile Towlette 100 Bx Soap Towlette) can be ordered using FHA Order# 468748.
-
Would a Level 3 mask last longer than a Level 1 mask during showering/bathing tasks?
No, using a level 3 mask would not mean the mask capability will last longer.
The moisture/steam generated during a shower/bath, would go into the mask through the path of least resistance, meaning the sides of the mask. This can easily saturate the two inner layers of the mask causing decreased filtration capability. This saturation would be the same regardless of the level of mask used.
-
Do I need to wear a respirator (e.g. filtering facepiece respirator N95 or equivalent) with all COVID-19 patients?
Don a respirator (e.g. FFR (N95) or equivalent, or EHFR) to which you have a current fit-test (in last 12 months) if providing care to a patient on airborne precautions. In addition, use a respirator if Point of Care Risk Assessment indicates a higher risk of transmission of COVID-19:
- Patient undergoing AGPs
- In a room or unit with multiple patients who are suspected or confirmed to have COVID-19 (e.g., cohort unit or COVID-19 test collection and assessment centres)
- If there is prolonged close proximity (e.g., more than 15 minutes of face-to-face contact) to the patient
- If the patient has excessive and sustained coughing without wearing a medical mask for source control
- If it is anticipated that the patient will be doing an activity with heavy expiratory exertion (e.g., shouting and singing)
- In a room that is crowded or confined
-
What is the difference between a medical-grade/surgical filtering facepiece respirator (3M 1860/1870+) and a commercial-grade N95 respirator (e.g. 3M 8210)?
Commercial- and medical-grade filtering facepiece respirators (FFRs) (e.g. N95s) are of similar structure and design, the main difference between them is that commercial FFRs aren’t tested for fluid resistance. All FFRs (N95 or equivalent) are equally effective at filtering particles and providing protection against airborne infectious disease such as during an aerosol generating procedure.Fluid resistance is necessary for procedures that may generate high-pressure streams of liquid.
The commercial grade FFRs are approved for use in health care settings by Health Canada. If you have been fit-tested to a commercial grade FFR model such as 3M 8210 and are working in an operative or procedural setting conducting tasks that pose a risk of high pressure fluid splashes or sprays use the FFR in combination with a faceshield. In the event your FFR does become contaminated with blood or body fluid follow standard practice of stepping out of the patient room, doff and replace your FFR.
-
What is the difference between eye and facial protection?
All Fraser Health staff, physicians, and contracted staff working in patient care areas are required to wear eye protection. Eye protection helps prevent staff from touching their eyes and prevents droplet from entering their eyes.
Eye protection refers to PPE that protects the eyes, which includes safety glasses, goggles, and face shields. In general, eye protection are used when there is a potential for exposure to hazards involving the eyes (e.g. particulates, laser, BBF splash). Specific eye protection standards may vary depending on the hazard. Face protection refers to PPE that protects the face (including the eyes), such as face shields. These are used if both eyes and face protection are required (e.g. AGP).
-
Are safety glasses and goggles equivalent?
No.
Safety glasses allow air in and around the eye area due to small gaps. They are designed to fit firmly but not tightly around the eyes.

Safety goggles include a strap to secure the goggles over your eyes and fit tightly against the face to form a seal around the eyes. As goggles are larger and heavier, they may affect the fit of respirators when used together. Staff are required to be fit tested with the goggles on to ensure the fit of the respirator is still adequate.
Some goggles have an indirect venting system to prevent fogging. These have vents that are angled away from the front lens of the goggles to keep the risk of splashes from entering the goggles low.


-
What are the pros and cons of safety glasses vs goggles vs face shields?
Safety glasses
Goggles
Face Shields
Pros
-
Light weight
-
Comfortable to wear
-
Minimal gaps around the eyes
-
Covers majority of the face
-
Fits everyone
Cons
-
Gaps around the eyes
-
Does not cover the rest of the face
-
May slide away from the face when bending forward (fit dependent)
-
Limits peripheral vision
-
Heavy and less comfortable
-
Does not cover the rest of the face
-
Require staff to repeat fit-test with the goggles on
-
Gets warm
-
Gap below the chin
-
-
When should I be using safety glasses, goggles and/or face shields?
Safety Glasses
Goggles
Face Shields
When to wear
-
Everyday use in patient care area
-
Hazard includes dust or gas
-
AGP (besides intubation)
-
AGP (including intubation)
-
Everyday use in patient care area
-
Other tasks that may cause more droplet/sprays
Additional PPE required
- Tasks cause glasses to slip
-
Staff must come into close proximity with patient’s breathing zone
-
AGP
-
Other tasks that may cause more droplet/splash
-
Intubation
-
Other tasks that may cause more droplet/splash
-
N/A
Please note: Prescription glasses are not equivalent to safety glasses.
-
-
Are my safety glasses and goggles up to Fraser Health standards?
All safety glasses/goggles used within Fraser Health for droplet and other BBF protection must meet one of the following standards: 1) CSA Standard CAN/CSA-Z94.3-07 or Z94.3-15, Eye and Face Protectors, or 2) ANSI Standard ANSI/ISEA Z87.1-2015, Occupational and Educational Personal Eye and Face Protection Devices. In addition to the CSA/ANSI requirement, please ensure you choose safety glasses or goggles which fit you. Please refer to the BCCDC Eye Protection Fit Tool for more information: Eye_Protection_Fit.pdf (bccdc.ca). If your safety glasses/goggles satisfy all the conditions above and are in good conditions, they are up to Fraser Health standards.
-
I need to perform a task that requires the use of a respirator and have not been fit-tested in the last 12 months. What should I do?
Do not proceed and notify your supervisor/manager.
-
I am a health care worker and do not know my respirator (e.g. FFR N95 or equivalent) fit-test status. What should I do?
Refer to the Fraser Health Self Look-up Report to determine your current status. (Internal link - opens in new window when signed in to Fraser Health network)
-
I need a fit-test. How do I get fit-tested?
You have two options:
(internal links; you will need to be signed in to Fraser Health's internal network to access)- Have your department-trained fit-tester (if applicable) complete a fit-test for you.
- Use the online booking tool to schedule your fit-test during a Health and Safety fit-test session (You will need to be use Google Chrome or Microsoft Edge browsers)
