Frequency
- Latent stage: every hour
- Active first stage of labour and passive second stage: every 15-30 minutes
- Active second stage: after every contraction and minimum q5min
Indications
- Health term (37+0 - 41+6 weeks) women without risk factors for adverse perinatal outcomes and with normal uterine activity (no tachysystole or prolonged contractions)
- Normal intrapartum course with absence of:
- PV bleeding
- Meconium
- Dystocia
- Abnormal maternal VS
(PSBC DST2)
- Other common indications:
- Before:
- Amniotomy
- administration of medications
- transfer or discharge of patient
- After:
- admission of patient - establish baseline
- artificial or spontaneous rupture of membranes
- vaginal examinations
- administration of medications
- Before:
- Intermittent auscultation in specific clinical situations:
- Epidural analgesia
- Every 5 minutes for 30 minutes after the initial epidural dose and after any additional bolus top-ups of concentrated local anaesthetic
- A drop in maternal blood pressure required EFM
- Patient-controlled epidural analgesia (PcEA) uses a more diluted local anaesthetic and opioid solution and hypotension is rarely a problem. For this reason, self-administered top-ups do not require q5min auscultation.
- Post-dates (410-416)
- When returning in active labour following cervical ripening, or in spontaneous labour, with no risk factors
- After 413 weeks gestation, with normal non-stress tests (NSTs) and amniotic fluid volume
- Epidural analgesia
Technique
Both handheld Doppler and Electronic Fetal Monitor transducers can be used for IA. Digital display of the FHR on either of these devices can be a source of verification of the counted FHR.
When using EFM transducers the data archiving system and paper printing should be turned off to prevent subsequent retrieval and analysis of uninterpretable data (Use “maternal mode” on CPN).
Establish baseline:
- Leopold's maneuver's
- Place Doppler over the fetal back or shoulder
- Angle the transducer to find fetal heart sounds (compared to a 'galloping horse') rather than the fetal vessel sounds ('whoosh')
- Listen to fetal heart rate and palpate maternal pulse at the same time to differentiate
- Count fetal heart rate continuously for 60 seconds, between uterine contractions
- Repeat the 60 second count if accelerations or decelerations are perceived
- Record the baseline (with no accelerations or decelerations included) as a single number
- Re-establish baseline when:
- Change in fetal heart rate - increasing or decreasing rate during ongoing assessment
- Handover
- Isolated maternal fever or tachycardia
Ongoing intermittent auscultation (IA) technique
- Explain procedure to the mother, emphasizing that fetal heart rate is taken immediately after the contraction
- When the end of the contraction is perceived by the mother and by palpatation, place Doppler over the fetal back or shoulder
- Angle the transducer to find fetal heart sounds (compared to ‘galloping horse’) rather than fetal vessel sounds (‘whoosh’)
- Place one hand on the uterus to palpate contractions and/or fetal movements
- Palpate the maternal pulse, if needed, to differentiate fetal heart
- Count in 6 second intervals for a total of 30-60 seconds
- Multiply 6 second counts by 10
- The 6 second count allows identification of accelerations and decelerations
- Fetal heart rate (FHR) without accelerations or decelerations is documented on the graphic section of the partogram, and accelerations and decelerations are indicated by √ below the graph
- For example: in a 60 second period there may be six 6- second counts: 13, 14, 13, 16, 15, 13 – the fetal heart rate (FHR) would be documented as 130 or 135 and accelerations √
Interpretation
- Fetal heart rate
- Rhythm (regular or irregular)
- Presence of acceleration
- Presence of deceleration
Classification normal
- Baseline rate range 110 to 160 bpm; fetal heart rate matches baseline range following contractions
- Regular rhythm
- Presence of accelerations - absence of accelerations does not make the interpretation “abnormal”
- Absence of decelerations
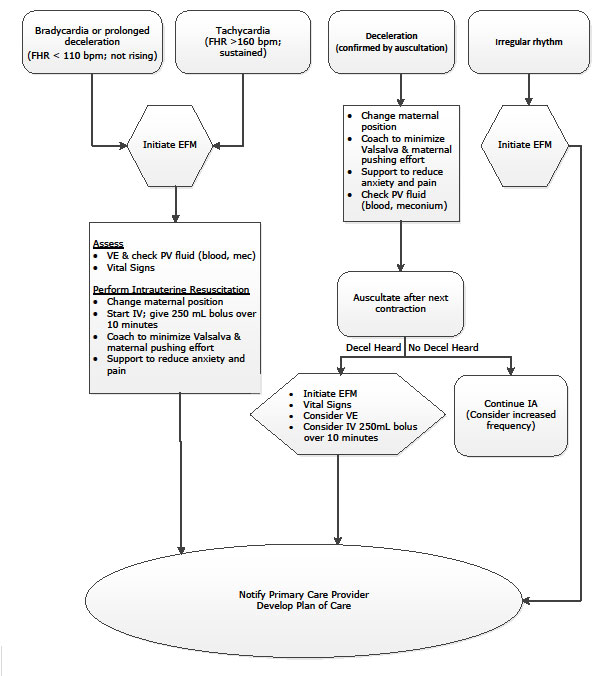
Classification abnormal
- Baseline rate
- Tachycardia (FHR > 160 bpm)
- Bradycardia (FHR < 110 bpm)
- Changing fetal heart rate baseline
- Increasing or decreasing fetal heart rate baseline detected over time
- Irregular rhythm
- Presence of decelerations
Communication - baby pause for intermittent auscultation
Baby Pause
Primary nurse report:
- □ Existing RISK FACTORS
- □ Additional RISK FACTORS developed in labour
- □ Location of fetal back
- □ Contraction pattern > □ Frequency □ Duration □ Intensity □ Resting tone
- □ Baseline rate
- □ Time baseline rate established
- □ Maternal pulse rate
- □ Rhythm
- □ Presence of decelerations and actions taken
- □ Presence of accelerations
- □ Classification > □ Normal □ Abnormal
Primary nurse and incoming care provider
- □ Establish management plan
- □ Document in chart