Providing situation updates and guidance on several vaccine preventable diseases to assist your practice.
Please encourage your patients to update their immunizations and their family’s immunizations, and take steps to ensure early diagnosis, isolation and treatment where possible. To book immunizations, please call:
- 604-702-4906 for residents of Fraser East communities (Mission, Abbotsford, Chilliwack, Agassiz and Hope)
- 604-476-7087 for residents in other areas of the Fraser Health region
1. Invasive group A streptococcus
Situation: Incidence of invasive group A streptococcal infections (iGAS), caused by streptococcus pyogenes, has been increasing in B.C., particularly among children. Incidence of emm type 1, associated with severe disease, has increased from 0.9 per cent of isolates in 2022 to eight per cent in 2023.
Case presentation: S. pyogenes infections typically causes tonsillitis, pharyngitis, impetigo, erysipelas, scarlet fever and cellulitis. It can also cause severe invasive complications such as sepsis, pneumonia, necrotizing fasciitis, toxic shock syndrome, acute rheumatic fever and post-streptococcal glomerulonephritis.
Clinical guidance: When assessing patients with acute respiratory illness or skin and soft tissue infections, please consider possible iGAS infection if:
- Prolonged fever of five or more days in a child of any age, or fever of any duration in a child younger than three months
- Fever with diffuse sandpaper rash, or rash that appears like sunburn or strawberry tongue
- Warning signs: Respiratory distress with nasal flaring, shortness of breath; very sleepy or having difficulty waking up; or when the child becomes very sick, very quickly
Testing: Please consider throat swab testing when there is diagnostic uncertainty and send to the emergency department for a full work up if there are concerning signs.
Prevention:
- There is no specific vaccine for S. pyogenes. Staying up to date with immunizations including varicella, influenza and COVID-19 can reduce risk of secondary infection.
- Prevent secondary cases: Please work with local public health, who will investigates all cases of iGAS, identify close contacts and recommend chemoprophylaxis to close contacts of severe iGAS.
2. Measles
The World Health Organization (WHO) has reported a 79 per cent increase in the number of global measles cases in 2023 compared to 2022. The chief public health officer of Canada has recently issued strong advice to everyone in Canada to be vaccinated with two doses of a measles vaccine, especially before traveling.
Clinical presentation: Measles, caused by the measles virus, presents with a two to four day prodrome of fever, coryza, cough, conjunctivitis, followed by a maculopapular rash three to seven days after symptom onset. The rash begins on the face and spreads over body, sometimes desquamates and lasts four to seven days.
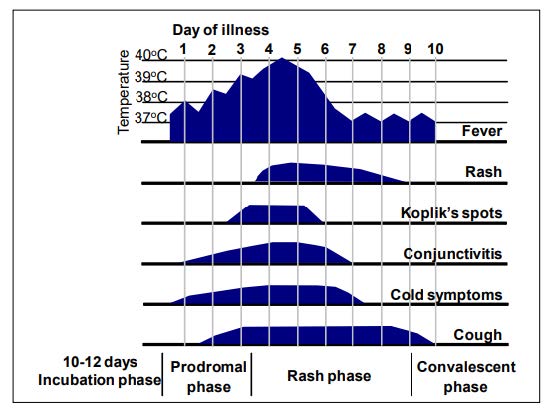
Figure 1. Clinical course of primary measles infection
Source: Manual for the laboratory diagnosis of measles and rubella virus infection. 2nd Ed. WHO (2007). https://www.who.int/publications/i/item/WHO-IVB-07.01
Testing: Diagnostic work-up of probable and suspect cases should include both serology and virus detection by nasopharyngeal swab and urine sample (using RT- PCR testing).
- Nasopharyngeal (NP) swabs for PCR can be collected up to eight days after rash onset.
- Urine samples for PCR may be collected up to 14 days after rash onset.
- Please identify the blood sample for IgM and IgG serology as “acute measles” on the lab requisition and obtain the first (acute) sample at the time of presentation and no later than day seven following rash onset. As the clinical presentation of measles can resemble other viral infections, please request that sera from suspect cases of measles be tested for antibody to parvovirus B19 and rubella.
- Please note that 20 per cent of measles cases will not have a reactive IgM when blood is drawn within the first three days of rash. For this reason, a second blood sample is indicated if the IgM serology results from an early acute phase sample are inconclusive or negative for measles, rubella and parvovirus B19, and the person meets the clinical case definition for measles.
Prevention:
- MMR or MMRV vaccines provide protection against measles. The efficacy of live measles vaccine is estimated to be 85 per cent to 95 per cent for one dose and 100 per cent for two doses.
- Public Health will identify close contacts for whom immunoprophylaxis is recommended. Immunoprophylaxis would be more effective if we are able to reach contacts within six days of exposure to the case so prompt notification to public health is appreciated.
- Immune globulin can prevent measles disease in people exposed to measles but who are unable to be immunized with vaccine due to contraindications.
- Travel and measles vaccine: Infants six to 12 months of age, traveling to countries where measles disease is common, should receive a dose of measles, mumps, rubella (MMR) vaccine early. These children will need two more doses of the vaccine after their first birthday. (HealthLink BC and chief public health officer of Canada advice).
3. Haemophilus influenza serotype b (Hib) infections
Situation: According to the BCCDC, since 2020, an increase of invasive Haemophilus influenzae type b (Hib) has been observed among adults in British Columbia. The majority of cases are adults experiencing homelessness and those with a substance use disorder. Pediatric incidence has not increased in parallel.
Clinical presentation: The bacteria Haemophilus influenzae serotype b can cause disease such as meningitis, pneumonia, cellulitis, osteomyelitis, septicemia, septic arthritis, empyema, pericarditis and epiglottitis.
Testing: Please consider haemophilius influenzae in the differential for patients presenting with serious illness including meningitis, epiglottis, pneumonia or septicemia. Depending on symptoms observed, please test epiglottis and normally sterile site, such as cerebrospinal fluid, blood, pleural fluid or joint fluid for Hib via PCR and culture.
Prevention:
- Hib vaccines can help protect against Hib infections.
- Public health will identify close contacts for whom chemoprophylaxis +/- immunoprophylaxis is recommended. Chemoprophylaxis should be initiated as soon as possible, ideally before 14 days have passed since last contact with the index case so early notification is appreciated.
4. Mumps
Situation: The 2021 childhood National Immunization Survey shows decline in mumps vaccine coverage for two doses of mumps-containing vaccine. Adequate protection against mumps virus requires not just one but two doses of vaccine.
Clinical presentation: Mumps is caused by the mumps virus. It commonly presents with fever, headache, and unilateral parotitis and sialadenitis. It can also cause epididymo-orchitis in males and oophoritis in females, presenting as abdominal pain. About one in five patients with mumps can also be asymptomatic, and one in three without characteristic sialadenitis.
Testing:
- PCR is preferred:
- Within the first three to five days of parotitis or other mumps symptoms, please collect a buccal swab or saliva from the buccal cavity.
- Over five days after symptom onset, please collect a urine specimen for RT-PCR.
- Serology:
- In all cases, please collect both acute and convalescent serum specimens for mumps serology.
- The first (acute) serum sample should be collected as soon as possible upon suspicion of mumps and within five days after symptom onset.
- If mumps IgM class antibody is not detectable in a mumps compatible case, the blood may have been drawn too early. Please collect another sample for retesting.
- The second (convalescent) serum should ideally be collected at least 10 days and up to three weeks after the first sample. Please refer to prior medical health officer update for more details on mumps testing.
Prevention: MMR or MMRV vaccines provide protection against mumps. Immunized individuals are far less likely to get mumps. Even if they develop mumps infection, are much less likely to experience complications.
Pertussis (“whooping cough”)
Situation: Several outbreaks of pertussis, a serious but preventable bacterial infection, have been identified across Canada in recent years.
Clinical presentation: Pertussis, caused by the Bordetella pertussis bacteria, can presents at various stages.
- Catarrhal stage (usually one to two weeks): Nasal congestion, runny nose, sore throat, dry cough, minimal or no fever.
- Paroxysmal stage (usually one to six weeks, up to 10 weeks): Dry cough changes to repeated bursts of numerous bouts. It may end with inspiratory “whoop” or post-tussive vomiting in children.
- Convalescent stage (usually two to six weeks but may be longer): The severity of illness wanes and the frequency of coughing bouts decreases.
- Infants younger than six months of age may experience atypical disease: With gagging, gasping or apnea as early manifestations; absence of whoop; and prolonged convalescence. Adolescents and adults may also experience atypical manifestations, i.e. cough is not paroxysmal or “whooping”.
Testing: Please collect NP swabs or NP wash as per instructions from the eLab Handbook.
Prevention:
- Age appropriate DTaP and Tdap vaccines protect against pertussis. Neither vaccination nor natural disease confers complete or lifelong protective immunity against pertussis or re-infection. Immunity wanes after five to 10 years from the last pertussis vaccine dose.
- Public Health will identify close contacts for whom chemoprophylaxis is recommended.
Please review your patients’ vaccine history and refer to Public Health for vaccination. In all cases, please encourage your patients to practice good hand hygiene; avoid sharing food, utensils, drinking glasses, bottles, soothers or toys; and cover coughs and sneezes with a tissue or forearm.
