Find resources to deal with this serious lung disease.
Short of breath?
You could have Chronic Obstructive Pulmonary Disease (COPD), a chronic lung disease that often goes undiagnosed. Smokers or ex-smokers over 40 are at the highest risk.
COPD is a lung disease that includes respiratory disorders such as chronic bronchitis and emphysema. About 138, 500 people in BC and 30, 000 people in Fraser Health live with COPD. More than 10,000 new cases were reported last year in the province. Many people do not know they have COPD until they experience an acute episode.
Think you may have COPD?
If you are over 40 and smoke currently, are an ex-smoker, or have been exposed to lung irritants, you may have COPD. Non-smokers can also get COPD. We recommend you take the 30-second lung health test below.
- Do you cough regularly?
- Do you cough up mucous/phlegm frequently?
- Do even simple chores make you short of breath?
- Do you wheeze when you exert yourself (exercise/go upstairs)?
- Do you get many colds, and do they last longer than your friends’ colds?
If you answered yes to one or more of these questions, you may have symptoms of COPD. Please see your primary care provider for your symptoms.
Please note: This test is intended for informational purposes only. It should not be used to replace advice, treatment, or diagnosis given by your primary care provider.
-
What does COPD mean?
COPD stands for Chronic Obstructive Pulmonary Disease
COPD occurs when your airways are exposed to pollutants such as smoke from cigarettes, fire or other irritants, they become inflamed, red and swollen.
Your airways then become filled with thick sticky mucous that you need to cough to clear the mucous. This mucous stays stuck in your airways, often blocking the airflow and trapping air.
The airways branch into smaller and smaller tubes, which end in millions of air sacs, called alveoli. The alveoli exchange air. Your alveoli can also be damaged and destroyed by these irritants, resulting in poor air exchange and the loss of elasticity trapping air in the lungs.
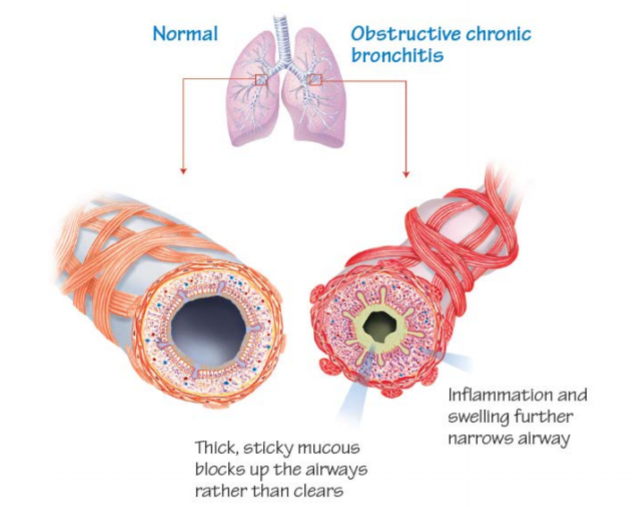
Image credit: Living Well with COPD™

Image credit: Living Well with COPD™
-
How is COPD diagnosed?
A breathing test known as spirometry is required to diagnose COPD.
During this test, a client will take a big breath in and blow all the air out into a tube attached to a machine.
The more blocked the airways are, the longer it will take to blow all the air out.
Image credit: Living Well with COPD™
-
What are the common signs and symptoms of COPD?
The most common symptoms of COPD are:
- Shortness of breath
- Cough
- Mucous production
-
What can I do to manage my symptoms?
- Quit smoking
Smoking is one of the primary causes of COPD and the main factor for its progression. Quitting smoking is the best thing someone with COPD can do for their health. To learn about services and resources to help you quit smoking, please visit our Quitting smoking page. - Respiratory Rehabilitation Programs
There are community and hospital-based programs throughout Fraser Health that offer education on lung health, wellness and exercise. Your primary care provider can refer you to our programs. These programs are now being offered virtually. For more information, please visit our Lung Health or Community Respiratory Services pages. - Immunizations
People with COPD are at a higher risk of complications from the flu and pneumonia. Please talk to your primary care provider to ensure your vaccinations are up to date. To learn more about immunizations, please visit our Immunizations section.
- Quit smoking
-
What treatment is available for COPD?
COPD can not be cured, but it can be treated so you can live a fulfilling life.
The best treatment includes quitting smoking, taking your COPD medications as prescribed by your primary care provider, staying active, and preventing and treating flare-ups early.
Medication can help improve your symptoms and quality of life.
You should always know the following about your medication:
- the name of each medication you are taking
- what your medication does
- the dose you should be taking
- when you should be taking your medication
- how to take your medication properly
- the precautions and side effects of the medications you are taking
It is important to take them regularly and as prescribed. Your primary care provider can help you to acquire a better routine to take your medications on a regular basis.
If you have any concerns or questions about your medications, please contact your primary care provider or pharmacist.
For more information on medication types, please read pages 9 to 19 of the Living Well with COPD™ - A plan of action for life summary guide.
You can find how-to guides for different inhalers below:
- Handihaler
- Genuair
- Breezehaler
- Respimat
- Diskus
- Turbuhaler
- Ellipta
- Metered Dose Inhaler (MDI)
- Metered Dose Inhaler with Spacer
Read our guide on telemonitoring to help you manage your health from home.
-
How do I know when I'm having a flare-up and what should I do?
Flare-ups or COPD exacerbations are when there is an increase in symptoms from your usual.
It is very important for you to know what your normal symptoms are so you can be aware of when they change. Discuss a flare-up plan with your primary care provider and they will prescribe medications and explain to you how to manage your flare-up.
Most flare-up plans follow a street light path:
- Green - Your COPD is well controlled and your symptoms are in their usual state, you continue to use your medications as prescribed by your primary care provider.
- Yellow - Your symptoms are worse. Take Action. There are some changes in your symptoms and your medications need to be adjusted. Your primary care provider will provide clear directions on what actions you should take.
- Red - Danger! Take action and get help. This is a medical emergency, call 911 or go to your nearest emergency department.
You can also download and print your own COPD Flare-Up Action Plan.
-
Are there any educational handouts for COPD?
Yes, we have education handouts available for COPD.
Resources
- Canadian Lung Association
Information about respiratory conditions for both patients and the general public. - BC Lung Association
Resources and prevention information on lung health. - Living well with COPD
Designed to help physicians and health care professionals develop a partnership with their patients to help with the self-management of their disease. - Health Literacy and Chronic Disease Management
Videos on COPD available in English, Mandarin, Tagalog, Korean, Farsi, Cantonese, Filipino, Punjabi.
