Should I bring my child to the emergency room?
Reviewed December 2025.
Most parents have asked this question. Here are some guidelines around when to treat illnesses at home and when to seek emergency care.
-
Fever
Any temperature above 38°C is considered a fever. A fever is only a symptom, not a disease. The most common cause is an infection caused by a virus or by a bacteria.
With a high temperature, a child will feel unwell. They may not want to eat, be a little more fussy than usual and play less, but the fever will typically go away in 3-4 days.
A child with specific symptoms, such as an earache that lasts for more than two days, breathing problems or bladder symptoms along with the fever, should be assessed by their family doctor. As well, babies younger than three months old with fever should be urgently seen by a doctor.
How can a parent help?
Along with rest, make sure they drink enough fluids, even if it’s just sips of water or formula or more frequent breastfeeding. Use medications such as acetaminophen (Tylenol) and ibuprofen (Advil and Motrin) if you have them on hand. The right dosage depends on the age and weight of the child.
No fever-reducing medication?
If you are trying to treat a fever without fever-reducing medication, please try these steps:
- Have your child drink plenty of fluids
- Dress them in light clothing
- Sponge them with cool/tepid water
Please note:
- The emergency room does not have samples or take-home medications such as Tylenol and Advil.
- The emergency room cannot expedite referrals to specialists
When to seek help?
Parents should recognize symptoms that may represent a more serious underlying cause for the fever and know when to go to their family doctor or to the Emergency Room if their doctor is unavailable to see them quickly.
The degree of temperature is less important than the associated symptoms. Children with a fever who should be assessed by a doctor – their family doctor or an emergency room physician – as soon as possible include:
- Babies younger than three months. They can get very sick quickly and require an aggressive approach to investigate the underlying cause.
- Children who experience seizures due to a rapid increase in temperatures.
- Children with a fever for more than three days.
- Children whose temperature repeatedly rises above 40°C
- Children with a known chronic medical condition.
- Children with a new rash.
- Children who are clearly quite unwell – lethargic, listless, rapid breathing, not drinking, poor interaction, inconsolable.
Visit HealthLinkBC for more information about fevers.
-
COVID-19, Influenza and RSV
COVID-19 symptoms can range from mild to severe. Sometimes symptoms start as mild and then suddenly worsen after a few days. Symptoms can include: fever or chills, cough, loss of sense of smell or taste, difficulty breathing, sore throat, loss of appetite, runny nose, sneezing, extreme fatigue or tiredness, headache, body aches, nausea or vomiting, diarrhea. Learn what to do if your child tests positive for COVID-19.
Flu symptoms can include fever, headache, muscle pain, runny nose, sore throat, extreme tiredness, and cough. Although colds and other viruses may cause similar symptoms, those due to the influenza virus tend to be worse. Fever and other symptoms can usually last 7 to 10 days, with the cough and weakness lasting up to two more weeks. In children, gastrointestinal symptoms such as nausea, vomiting and diarrhea may accompany the respiratory phase.
Respiratory Syncytial Virus (RSV) is a common cause of respiratory illness in infants. It causes nasal congestion, coughing, wheezing and mild fever. Symptoms peak on the fifth day of illness but improve after. However, a cough may last for three to four weeks. There is no treatment and most infants spontaneously improve. Some may require supportive treatment with oxygen and hydration. RSV may have a more serious impact on infants less than 6 weeks old or those born prematurely.
How can a parent help?
Help your child manage their symptoms by encouraging them to drink plenty of fluids and get lots of rest. You can use a humidifier or hot shower to help ease a cough or sore throat. If they have a fever, you can use non-prescription medicine like children’s Tylenol or children’s Advil.
When to seek help?
Seek emergency help for your child if they:
- find it hard to breathe
- have chest pain
- can’t drink anything
- feel very sick
- feel confused
-
Common cold
A cold is an upper respiratory (upper chest/throat/head) illness caused by a virus infection of airway passages. You know your child has a cold if they have a runny/stuffy nose, sneezing, watery eyes, sore throat, cough, aches, sweats, and/or a fever.
Colds are contagious during the first three to four days. Antibiotics will not help recovery because antibiotics cannot cure viruses.
How can a parent help?
With plenty of clear fluids (water, fruit juice, tea, clear soups), and rest, a child often recovers in a few days or sometimes in up to a week or two.
When to seek help?
- Unusual shortness of breath
- Not responding to you
- Child is clearly very unwell – lethargic, listless, not drinking at all, poor interaction, inconsolable
Most colds can be cared for at home or by a family doctor. If you feel your child is very unwell or Fraser Health Virtual Care or 8-1-1 recommends it, a visit to the ER may be appropriate.
-
Gastroenteritis (diarrhea and/or vomiting) aka stomach flu
Most diarrhea and/or vomiting in children is caused by a virus. Children with gastroenteritis, also known as stomach flu, may experience stomach cramping, fever, fatigue and lack of appetite.
Antibiotics will not help recovery because antibiotics cannot cure viruses.
How can a parent help?
If your child is being breastfed, continue even if the baby is unwell or has diarrhea. Feed them smaller volumes more frequently.
Be sure your child drinks to replace lost fluids. You can purchase Pedialyte (or Lytren/Gastrolyte) from a pharmacy. Older children can also have diluted juice and clear soup/broth.
After 24 hours of just fluids, the diarrhea and vomiting will likely decrease. If symptoms are improving, slowly return your child to their normal diet of formula or easily digestible solid food (crackers, flour chapati/roti, rice cereal, mashed potatoes, plain meat/eggs, applesauce, and bananas).
If the diarrhea is almost gone by day three, return your child to their normal food.
When to seek help?
- No decrease in the diarrhea after 24 hours of just fluids
- Signs of dehydration (dry mouth, severe thirst, no tears when crying)
- No urine for six to eight hours in older children or four to six hours for babies and young children
- Blood-stained mucous or stools
- Starting to appear more sick
- Has bad belly pain that lasts for more than a few minutes at a time
- Is not responding to you
Most cases can be cared for at home or by a family doctor. If you feel your child is very unwell or Fraser Health Virtual Care or 8-1-1 recommends it, a visit to the ER may be appropriate.
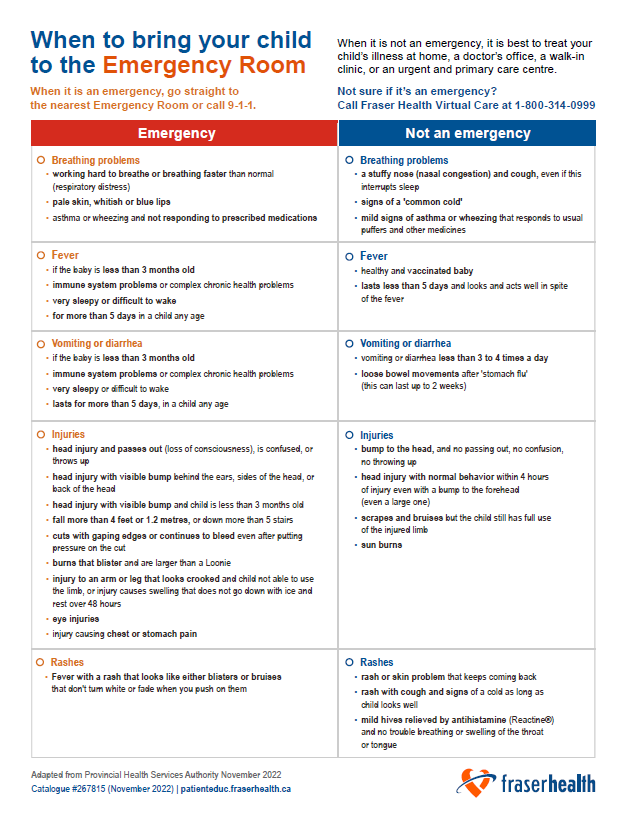
Examples of when to bring your child to the emergency room
Access the text in the graphic above:
-
Emergency
Breathing problems:
- respiratory distress (working hard to breathe or breathing faster than normal)
- pale skin, whitish or blue lips
- asthma or wheezing and not responding to prescribed medications
Fever:
- in a child less than three months old
- with immune system problems or complex chronic health problems
- very sleepy or difficult to wake
- for more than five days in a child any age
Vomiting or diarrhea:
- in a child less than three months old
- repeated vomiting and unable to keep liquids down
- vomiting or diarrhea containing large amount of blood
- vomiting bright green
- dehydration with dry mouth or no urine more than 12 hours
Injuries:
- head injury with loss of consciousness (passing out) or confusion
- head injury with visible bump behind the ears, sides of the head or back of the head
- head injury with visible swelling and the child is less than three months old
- fall more than 4 feet or 1.2 metres, or down more than 5 stairs
- cuts with gaping edges or continuing to bleed despite direct pressure
- burns that blister and are larger than a Loonie
- injury to arm or leg that looks crooked, causes inability to use the limb, or creates swelling that does not go down with ice and rest over 48 hours
- eye injuries
Rashes:
- fever with a rash that looks like either blisters or bruises that don't turn white or fade when you push on them
-
Not an emergency
Breathing problems:
- nasal congestion and cough (even if it interrupts sleep)
- symptoms of the 'common cold'
- mild asthma or wheezing that responds to usual puffers
Fever:
- in healthy and vaccinated babies
- in children who appear generally well
Vomiting or diarrhea:
- vomiting or diarrhea less than three to four times a day
- ongoing diarrhea after 'stomach flu' (this can last up to two weeks)
Injuries:
- minor head injuries (with no loss of consciousness, no confusion and no vomiting)
- mild head injuries with normal behavior within four hours of injury and bumps (even large) to the forehead
- scrapes and bruises where the injured part can still be used
- sun burns
Rashes:
- recurring rashes or skin problems
- rashes with cough and cold symptoms, if the child looks well
- mild hives that respond to antihistamines (Reactine®) without difficulty breathing or throat/tongue swelling
Prevention
There are also things we can all do to help prevent the spread of all respiratory illness this season. These include:
- Get all recommended vaccines including influenza and COVID-19 booster vaccine doses.
- Stay at home if you feel unwell and try to avoid spending time with people at higher risk of serious illness.
- Practice respiratory etiquette: wear a mask in indoor public spaces (if you choose), cough and sneeze in your elbow.
- Clean your hands regularly and avoid touching your face, especially your eyes, mouth and nose.
Critical or life-threatening conditions
Go to the emergency room or call 9-1-1 if your child has:
- a fever of 38 degrees (100.4 degrees F) or higher and is younger than three months old
- difficulty breathing
- severe abdominal or chest
- pain/pressure
- loss of consciousness
- heavy bleeding
- blue lips or skin, or appears very pale
- excessive vomiting, especially if there is blood in the vomit
- diarrhea and vomiting, lack of tears or urine over several hours
- high fever or lethargy, without improvement with acetaminophen (Tylenol) or ibuprofen (Advil)
- an injured swollen or crooked limb
- ingested a toxic chemical, including a
- suspected drug or alcohol overdose
Not sure if it’s an emergency?
- Call your family physician or primary care provider
- Call Fraser Health Virtual Care at 1-800-314-0999, from 10 a.m. to 10 p.m., or call 8-1-1 outside of those hours
- Visit an urgent and primary care centre: fraserhealth.ca/urgentcare
- For minor ailments, such as urinary tract infections (UTIs) and Pink Eye, and medication refills speak with your pharmacist.
Visit fraserhealth.ca/careoptions for more information.
View emergency room wait times.
Learn about moving through the Emergency and know what to expect when you arrive.