Staff at the provincial BC Biocontainment Treatment Centre at Surrey Memorial Hospital took part in the simulation to test their ability to respond to a high-threat pathogen.
From August 18 to 20, the simulation brought together a multidisciplinary team that included clinicians, registered nurses, paramedics, infection prevention and control, and provincial partners to prepare for the potential arrival of diseases such as Ebola, Lassa fever or even a virus not yet identified.
“This kind of training is about readiness,” said Tracie Jones, manager of the BC Biocontainment Treatment and Provincial Training Centre, who also supports Fraser Health’s emergency preparedness.
“We want to make sure that if this scenario ever becomes reality, we can protect the public, safeguard our staff and provide the best possible care.”
The provincial BC Biocontainment Treatment Centre at Surrey Memorial Hospital is the only facility in B.C. able to provide ongoing care for viral hemorrhagic fevers. With just two beds, it is a specialized but limited resource, and patients are transferred there for care. For pediatric patients, the team includes intensive care and infectious disease specialists with pediatric critical care training.
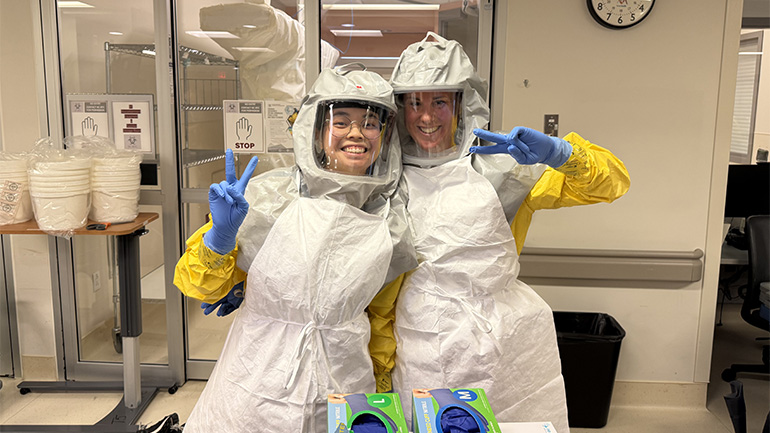
Day one of the simulation focused on building a strong foundation. Staff practiced getting into and out of personal protective equipment, rehearsed infection-control protocols and worked through the challenge of providing care while wearing full personal protective equipment. Tasks that usually felt routine, such as checking vital signs or preparing equipment, became more difficult under multiple layers of gloves and respirators.
The day also included a patient transfer scenario. While wearing full personal protective equipment, staff met BC Emergency Health Services paramedics outside the hospital, where a simulated patient had arrived in an EpiShuttle, a sealed transport pod. Together, they brought the patient safely into the hospital and up to the biocontainment treatment centre, practicing the steps required for a secure transfer without risk of exposure.
For many, including critical care nurse Erika Tsang, it was the first time participating in a simulation of a scenario with stakes this high.
“It takes at least two people to help each other into the gear,” she said. “You really rely on your colleagues. If one person misses a detail, another will catch it. That teamwork is what keeps us safe.”
Observers monitored every step of the simulation, flagging breaches or errors so they could be corrected on the spot.
“We do not get learning opportunities like this often,” Tracie said. “So, when we do, it is important to test the system fully and make improvements in real time.”
Day two built on this foundation as the simulated patient’s condition deteriorated, requiring life support. Staff practiced the complex process of providing critical care under strict biocontainment protocols, testing their ability to manage equipment and interventions while maintaining safety.
Day three concluded the simulation with a scenario in which the simulated patient passed away. This stage gave staff the chance to practice end-of-life protocols, including the sensitive but vital processes that follow. It was an opportunity to test not only technical skills but also communication and collaboration during one of the most difficult moments of care.
“Of course, I hope I never have to use this,” Erika said. “But if that day comes, I feel more prepared and more confident.”
At the end of the three days, teams reflected on what worked well, where improvements could be made and how the lessons learned would strengthen readiness across the province.


