Fraser Health and Simon Fraser University (SFU) have launched a pilot project to sequence the genome of Clostridioides difficile, a superbug responsible for severe infections.
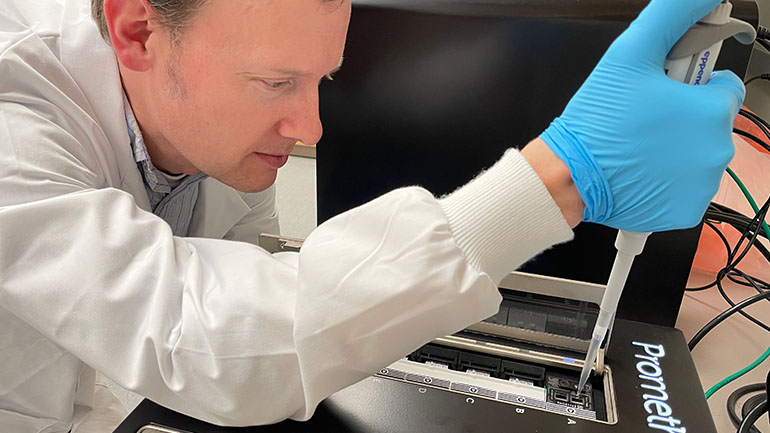
Photo: Dr. Michael Trimble, SFU genomics lab manager, places sample in advanced long-read sequencer for whole-genome sequencing.
Global epidemiologists recently raised the alarm over ‘nightmare bacteria’—germs that respond to only one or two medications because they’ve become so resistant to antibiotics.
Antimicrobial resistance occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medication. Infections then become easier to spread and harder to treat.
Clostridioides difficile infection (CDI or C. difficile) is one of the most common causes of infectious diarrhea in hospitals and long-term care facilities. The superbug usually attacks people who are immunocompromised or have been treated with antibiotics. It results in extended hospital stays, increased intensive care unit admissions and higher risk of mortality.
To better understand how patients acquire and transmit C. difficile, Fraser Health and SFU researchers are analysing the genetic makeup of C. difficile. Samples from infected patients at Abbotsford Regional Hospital and Cancer Centre are sent to SFU’s Department of Molecular Biology and Biochemistry. There, the samples are cultured and undergo whole genome sequencing—a process that involves extracting and decoding the DNA of the bacteria.
“We’re hoping to learn more about whether the C. difficile we see in our hospitals is transmitted from patient to patient or whether some patients are coming into hospital colonised with C. difficile,” says Dr. Kevin Afra, executive medical director for Antimicrobial Stewardship and Infection Control, Fraser Health. “Our hope is that this project will inform future antimicrobial stewardship and infection prevention strategies to enhance patient safety across the region.”
“Antimicrobial resistance is a major public health threat, and it needs collaboration across sectors to tackle this challenge,” says Dr. Amy Lee, Assistant Professor, Molecular Biology and Biochemistry, SFU. “Working closely with Fraser Health, we can provide detailed bacterial genomic information using advanced long-read sequencing technology to understand CDI transmission and resistance patterns in hospitals.”
Once the lab analysis is complete at SFU, the data will be integrated with Fraser Health’s epidemiological records to build a clearer picture of how C. difficile infection spreads.
“Through advanced computational analysis of the sequence data, we are able place the C. difficile from B.C. in the national and global context so clinicians can use these insights to improve local intervention strategies,” adds Dr. Will Hsiao, Associate Professor, Faculty of Health Sciences, SFU.
Fraser Health has robust infection prevention and control measures to protect patients, residents, staff, medical staff, volunteers and visitors from transmitting and/or acquiring infections. They include Highlight and Adenosine Triphosphate (ATP) testing. Combined with proper hand hygiene, appropriate precautions and cleaning, they reduce the risk of infections such as C. difficile, carbapenemase-producing organisms (CPO), Candida auris (C. auris) and methicillin-resistant Staphylococcus aureus (MRSA).
The pilot project is expected to run through the coming year, and the results will help us better understand how superbugs behave and spread in hospitals.
